Getting estradiol injections covered by insurance in Canada 🏳️⚧️💉🇨🇦
For a few months, I’ve been getting my HRT via injections, specifically estradiol valerate. It’s another option, like pills, patches, gels, and implants, which some people find better suits their situation, myself included. However, getting insurance coverage can be challenging, and I’ve heard many people, online and in-person, say it’s not possible.
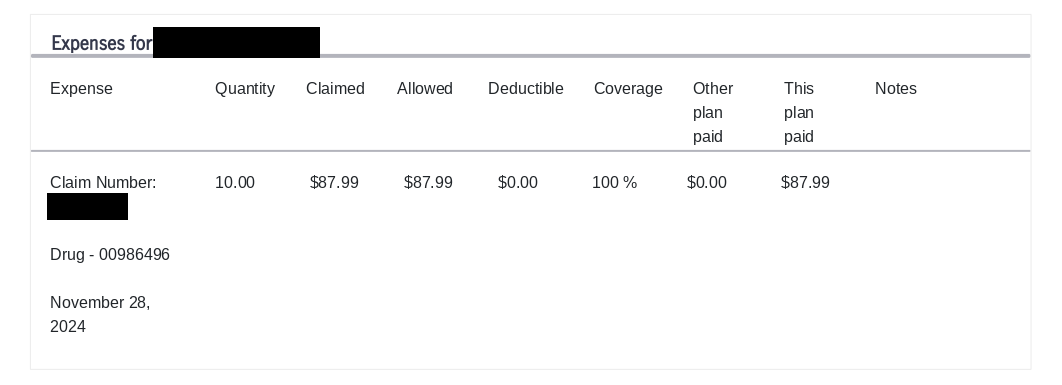
Today, I’m dispelling that rumour. For the last 3 months, I’ve gotten my prescriptions in Ontario consistently covered by Manulife. Here’s my most recent claim at the time of writing:
I’m sharing what I’ve learned, in the hopes that others will find success.
Background
So, first we need to understand why it’s so tricky to get estradiol injections in Canada.
The only form that’s approved is estradiol valerate. This was previously imported as brand-name Delestrogen (DIN 00029238) by the now-defunct Theramed Corporation until 2008, and a generic was available from Pharmascience until 2016 (DIN 00741930). Since then, there’s no way to purchase the commercially-manufactured version, so it has to be compounded by a pharmacy.
And this is where the problem arises. Compounded drugs don’t have their own DIN, so when you file an insurance claim, the company doesn’t recognize the prescription and denies it. Some compounded drugs instead have a pseudo-DIN, which isn’t registered with Health Canada, but the insurance companies recognize when processing claims. Unfortunately, estradiol valerate doesn’t have a pseudo-DIN. So, the challenge lies in translating the compounded drug to something they can recognize.
What to do
Before doing anything else, check if your provincial or territorial insurance already covers injections. It’s unlikely, but will save you a lot of stress if it is. For example, estradiol pills are covered under the Ontario Drug Benefit, but not injections, so I had to work with my group plan.
Your best chance of success is by filing a standard claim with a Drug Insurance Number (DIN). I talked to Manulife’s live chat1, and they recommended uploading the receipt for compounded drugs, but these got rejected half of the time. Still, it might be worth contacting the company and trying what they suggest. Don’t worry about resubmitting; I had to try 4 times with one receipt and never ran into any issues.
Here’s how to find the right DIN:
- Check the DIN provided on your prescription receipt (here’s an example). If it’s something like all zeroes or repeating digits, it’s probably a placeholder and won’t work. But otherwise, try using this first.
- Ask your pharmacy for the pseudo-DIN of the base “active” ingredient, estradiol. Your insurance may recognize this number in the claim.
- Finally, search for “<INSURANCE COMPANY> pseudo-DIN” and look for a chart of pseudo-DINs. Then, look for estradiol in the list.
Once you have the DIN, plug this into the claim details. When it asks for the quantity, use something that makes sense. Typically, estradiol valerate is compounded in Canada at a concentration of 10 mg/mL. So if you have a 5 mL vial, you could put the quantity as “5 mL” or “50 mg” (concentration times volume). If you have a different concentration, you should convert to milligrams and use that value, to make sure you receive the correct coverage.
What worked for me
My pharmacy provided me with pseudo-DIN 00986496 for the base ingredient. It also appears in an Express Scripts chart
under the name ESTRADIOL USP MICRONIZED. Using this, Manulife approved the claim and reimbursed me! Some findings:
- I’ve always filed my claims in mL. I’m not sure what results look like with mg.
- I originally had my estradiol compounded at my regular pharmacy. I got 2 mL for $84.14 (or $42.07/mL), plus an $11.99 dispensing fee. Manulife inconsistently reimbursed me for the full amount, but it was always a struggle.
- When I switched to my current method, they only covered $59.95. Subtracting the dispensing fee, this suggests Manulife will cover at a rate of $23.98/mL.
- After this, I switched to Pace Pharmacy. They compound 5 mL vials for $38, or $7.60/mL. Even with the $11.99 dispensing fee, Manulife can now cover the full amount.
It’s possible!
Hopefully this will help you find success, or at least increase your options. If you found this helpful, or know someone that this could assist, share the word!
